Keratoconus Specialist
In Katy, Texas
Understanding Keratoconus
Struggling with Keratoconus? We’re Here for You
Dr. Kauffman has been treating and managing patients with keratoconus for the past 12 years. Every patient with keratoconus is unique, some patients may achieve success with glasses or soft contact lenses while others may need to wear gas-permeable or scleral lenses to achieve optimal visual acuity. Dr. Kauffman takes the time to evaluate each individual patient with keratoconus and develops a customized treatment and management plan for that patient to provide the best visual acuity and quality of vision possible.
When it comes to dealing with conditions like keratoconus, having an experienced optometrist is crucial. Located right in Katy, Texas, Dr. Kauffman at Contemporary Eye Care is a renowned eye doctor with a track record of successfully treating patients with this condition. With expertise not just as an optometrist but also as a keratoconus specialist, Dr. Kauffman understands the intricacies involved in managing and treating this eye condition.
What is Keratoconus?
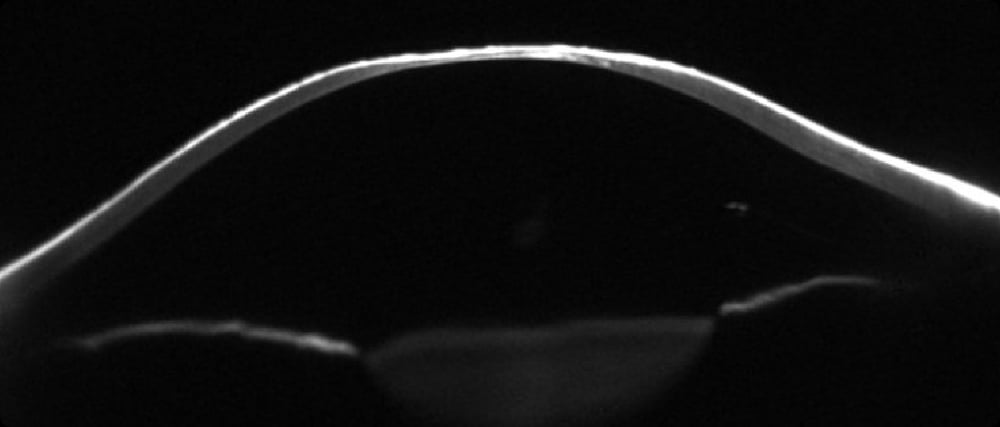
Keratoconus (KC) is a progressive eye disease that affects the shape and thickness of the cornea, causing it to bulge outward in a cone-like shape. This can cause visual distortions, such as blurred or double vision, and sensitivity to light. Although KC can cause significant vision changes, it does not cause permanent blindness. Keratoconus typically develops during the teenage years and progresses slowly over time, before stabilizing in the 30s and 40s. However, variations can occur. Some patients may not notice vision changes until their 20s or 30s while others may experience vision changes during early teenage years or even before.
Keratoconus is a considered bilateral condition, although one eye may experience more blur or distortions than the other.
Symptoms of Keratoconus
Keratoconus is a progressive eye condition that affects the shape and clarity of the cornea, the clear front part of the eye. It can cause distorted vision, sensitivity to light, and other visual disturbances. The symptoms of keratoconus can vary depending on the severity of the condition. Some common symptoms include:
• Blurred or distorted vision, especially at night.
• Double vision in one eye.
• Halos or glare around lights.
• Sensitivity to light.
• Eye redness and swelling
• Eye strain or fatigue
Causes of Keratoconus
The exact cause of keratoconus is unknown, but it is believed to be a combination of genetic and environmental factors. Some possible causes include:
- Abnormalities in the collagen fibers that make up the cornea
- Allergies or atopy – severe itching of eyes
- Genetics – family history of Keratoconus
- Certain medical conditions, such as allergies or connective tissue disorders
Diagnosing Keratoconus
Keratoconus can be diagnosed through a comprehensive eye exam, which may include:
- Visual acuity test: This measures how well you can see at different distances
- Refraction test: This determines your exact eyeglass prescription
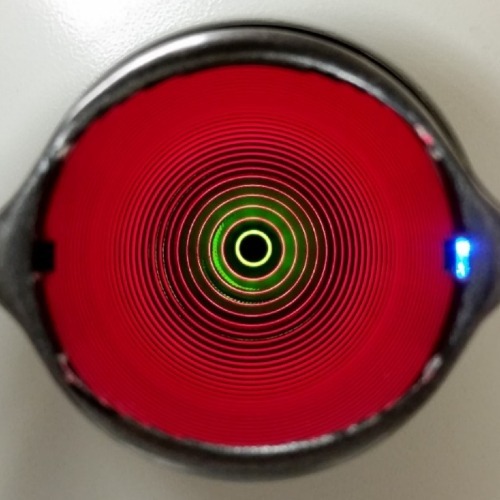
- Corneal topography (mapping): This measures the shape/curvature and thickness of the cornea
- Biomicroscope exam: A high-powered microscope is used to examine the cornea for signs of keratoconus
Keratoconus often develops during one’s teenage years, making regular eye exams essential. As an experienced eye doctor in Katy, Dr. Kauffman emphasizes the importance of these exams. Early detection can lead to more effective treatments and management plans tailored to the patient’s needs.
Treatment Options for Keratoconus
There are several treatment options available for keratoconus, depending on the severity of the condition. For those who require vision correction, Contemporary Eye Care provides an extensive range of contact lenses and treatments. Depending on your specific needs and the progression of your keratoconus, soft contact lenses or specialized scleral lenses might be recommended. Dr. Kauffman, a noted keratoconus specialist, ensures that patients receive the best fitting and most comfortable lenses possible.
Spectacles
Soft Contact Lenses
Specialty Contact Lenses
Scleral Lenses
Intacs/Corneal Transplant
Corneal Cross-Linking (CXL)
Living with Keratoconus
Living with keratoconus can be challenging, but there are coping strategies and support resources available to help.
Some tips for living with keratoconus include:
1. Follow your doctor’s treatment plan: This may include using eyeglasses or specialty contact lenses, or undergoing surgery.
2. Protect your eyes: Avoid rubbing your eyes, wear sunglasses to protect your eyes from UV radiation, and keep your eyes lubricated to prevent dryness.
3. Stay informed: Learn as much as you can about keratoconus and its treatment options. Ask us for additional information and resources.
4. Seek support: Join a support group (e.g. Facebook groups) or online community to connect with others who are living with keratoconus. Share your experiences, ask questions, and offer support to others.
5. National Keratoconus Foundation (NKCF): NKCF is a non-profit organization whose mission is to educate the public about keratoconus. Visit www.nkcf.org for more information.
Latest Research on Keratoconus
Researchers are constantly working to improve our understanding of keratoconus and develop new treatments.
Some recent studies have focused on:
- Using gene therapy to repair the damaged collagen fibers in the cornea
- Developing new surgical techniques, such as femtosecond laser-assisted corneal surgery, to improve the accuracy and safety of corneal transplant surgery
- Studying the role of environmental factors, such as UV radiation and oxidative stress, in the development and progression of keratoconus
Frequently Asked Questions
What is keratoconus?
Keratoconus is an eye condition where the cornea gradually thins and bulges into a cone-like shape. This irregularity affects how light enters the eye, causing distorted and blurred vision. At Contemporary Eye Care, we use advanced diagnostic tools to identify and manage this condition early.
What causes keratoconus?
While the exact cause remains unknown, genetic factors, chronic eye rubbing, allergies, and certain medical conditions are believed to contribute. Our comprehensive exams help identify potential risks.
What are the common symptoms?
Symptoms may include blurry or distorted vision, sensitivity to light, glare, and frequent changes in your glasses or contact lens prescription. If you’re noticing any of these, our team at Contemporary Eye Care can help evaluate and guide your treatment.
What treatment options are available?
Treatment depends on the severity of the condition. At Contemporary Eye Care, we offer a range of solutions, from custom contact lenses and scleral lenses to co-managing advanced treatment procedures such as corneal cross-linking. While we do not perform corneal cross-linking in-office, we work closely with trusted surgeons to co-manage the procedure and ensure seamless, comprehensive care. In more advanced cases, we may also coordinate referrals for corneal transplant surgery.
Is there a cure for keratoconus?
Although there is no cure for keratoconus, recent advances in technology allow keratoconus to be diagnosed earlier. With earlier detection, progression can often be managed effectively, decreasing the blurry or distorted vision.
Can keratoconus lead to blindness?
While keratoconus doesn’t typically cause complete blindness, it can significantly impair vision if left untreated. Advances in contact lens technology and designs, such as scleral lenses or wavefront guided scleral lenses, will often significantly improve vision in patients with keratoconus and improve the vision quality and reduce or minimize the distortions. Regular exams with our experienced optometrist will help prevent severe outcomes.
Who is most at risk?
It often develops in teens or young adults. Those with a family history, frequent eye rubbing, or chronic allergies may have an elevated risk. We recommend early screening for individuals in high-risk groups.
How often should I have my eyes checked if I have keratoconus?
Patients should visit every 6–12 months depending on the severity. At Contemporary Eye Care, we tailor follow-up schedules to your specific needs and ensure your vision is closely monitored.
How is keratoconus diagnosed at Contemporary Eye Care?
We use cutting-edge imaging technology, including corneal topography, pachymetry, and wavefront aberrometry, to map the cornea’s shape, thickness, and higher order aberration profile – allowing us to diagnose keratoconus in its earliest stages.
What is corneal cross-linking?
Corneal cross-linking (CXL) is a minimally invasive procedure designed to halt the progression of keratoconus by strengthening the corneal structure using UV light and riboflavin (vitamin B2). Our team can evaluate if you are a good candidate for this advanced therapy.
Testimonial From One of Our Keratoconus Patients
Keratoconus is a complex eye condition that can have a significant impact on a person’s vision and quality of life. However, with early diagnosis and appropriate treatment, many people with keratoconus, like our patient below, can manage their symptoms and maintain good vision!
If you are experiencing any symptoms of keratoconus, give us a call. We can recommend the best treatment options for your vision.
Keratoconus is a complex eye condition that can have a significant impact on a person’s vision and quality of life. However, with early diagnosis and appropriate treatment, many people with keratoconus, like our patient below, can manage their symptoms and maintain good vision!
If you are experiencing any symptoms of keratoconus, give us a call. We can recommend the best treatment options for your vision.
Schedule an Appointment
Are you ready to schedule your next appointment? Click the link below and fill out the necessary information and we’ll follow up with an appointment confirmation.
